Introduction
Common mental disorders include abnormal changes in mood, anxiety such as post-traumatic stress disorder, attention deficit disorder/attention deficit hyperactivity disorder, and autism. In addition, the four most common mental disorders that cause disabilities are depression, bipolar disorder, schizophrenia, and obsessive-compulsive disorder (OCD).1,2 To date, 58 million people in the US are diagnosed with some form of mental disorder, and this number is expected to increase over the next decades.3–5 Psychotherapy and applied psycho-pharmacotherapy do not always bring the expected results6; therefore, the search for alternative therapies and/or management strategies for these diseases is warranted.
In recent years, there has been a dramatic increase in research on the effects of food and nutrients on the prevention of many mental disorders, and researchers have observed that the prevalence of mental health disorders has increased in developed countries in correlation with the deterioration of the Western diet,7 which includes pre-packaged foods, refined grains, red meat, processed meat, high-sugar drinks, candy, sweets, fried foods, conventionally raised animal products, high-fat dairy products, and high-fructose products.8
From a health perspective, the Western diet, which consists of ultra-processed foods, may disrupt gut health and affect mood and mental well-being. These foods can promote inflammation, and inflammation is linked to increased levels of anxiety and stress in the body.9,10 Transitioning toward a diet comprising minimally processed, nutrient-dense foods can mitigate the deleterious effects of ultra-processed foods and promote microbial resilience, the capability of a microbial community to resist or recover from perturbations to its original state of balance.11 Furthermore, the incorporation of probiotics, prebiotics, and lifestyle modifications offers potential strategies for restoring gut homeostasis. In addition, staying hydrated can promote digestive function, and regular physical activity enhances gut motility.12
To reduce inflammation and improve mental health, consider incorporating whole grains like brown rice and quinoa for fiber and nutrients; lean proteins such as fish, chicken, and legumes to support brain function; and regular intake of antioxidants from fruits and vegetables, which can counteract the effects of inflammation and may alleviate anxiety and stress symptoms.13 The main goal of this review is to update knowledge nutritional influences on various mental issues and how the outcomes may have practical potential as alternative therapeutics and/or management options in real scenarios. Preclinical-to-clinical studies as well as meta-analyses were searched to gather evidence for conclusions regarding the role of nutrition in mental health.
A systematic literature search was conducted in Oct–Nov 2025 across several key databases, including PubMed, Google Scholar, and Web of Science, to identify relevant peer-reviewed articles. The search strategy utilized a combination of keywords and controlled vocabulary, MeSH terms (Medical Subject Headings).
Causative factors of mental disorders and their treatment options
Developmental disorders, the use of any psychoactive drugs, or trauma may cause psychiatric disorders. In addition, genetic predisposition could also be involved in the onset and progression of mental disorders. Early detection and treatment of psychotic disorders could result in a better response.14 Some biomarkers, like hypothalamic-pituitary-adrenal axis dysfunction with elevated cortisol levels, are linked to increased inflammation and oxidative stress.15,16 Pro-inflammatory cytokine levels are higher in psychiatric patients.17,18 The anti-inflammatory and antioxidant compound statins can reduce depressive disorders.19
This review aims to discuss, with scientific evidence, the effects of nutrition on mental health and disorders. Specifically, the focus is on:
Correlations between nutrition and mental health;
The psycho-protective effect of food, if any;
Scientific evidence of the preventive potential of food for mental disorders.
Correlations between nutrition and mental health and disorders
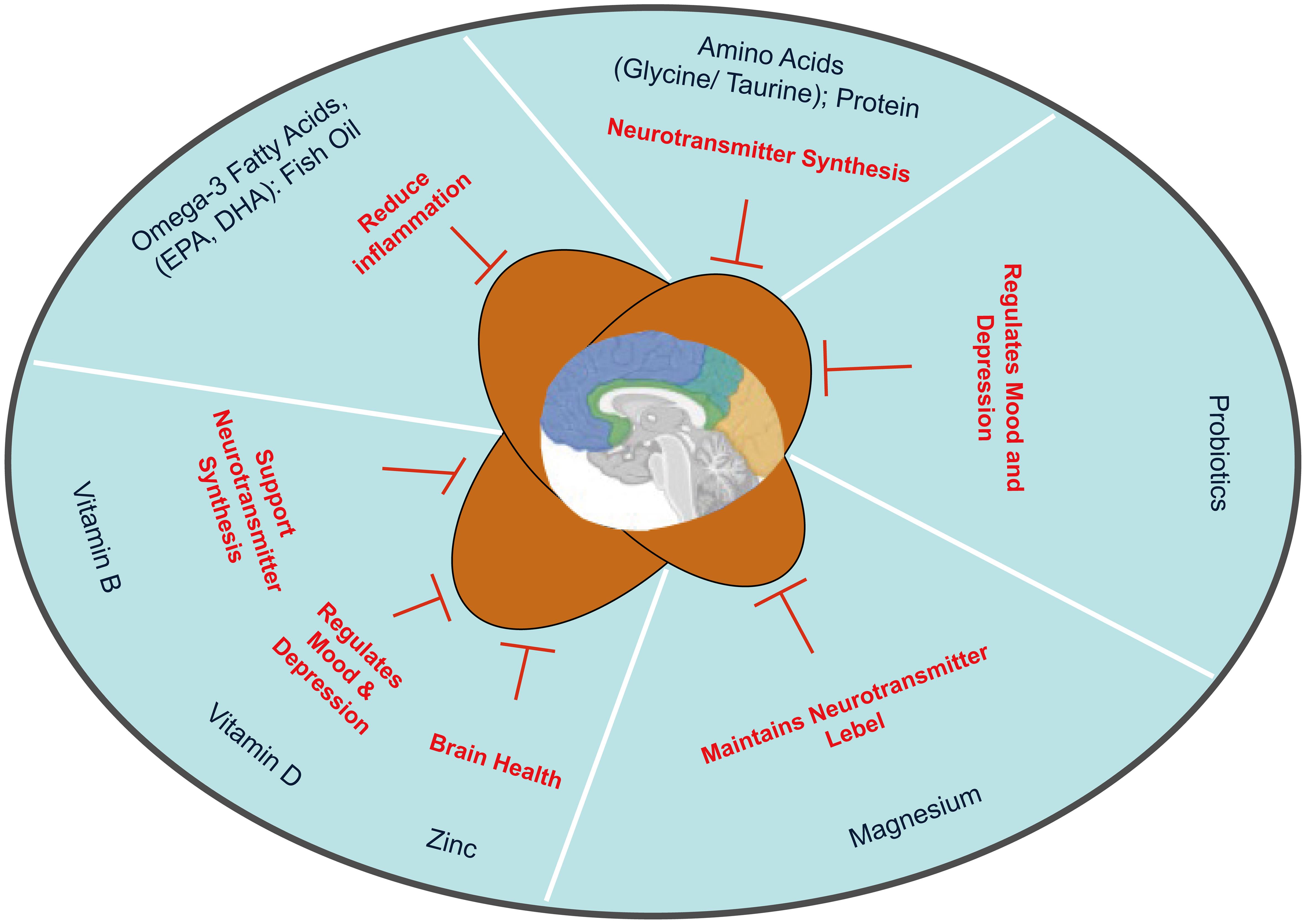
Various research studies highlight the connection between nutrition and mental health conditions such as depression, anxiety, and attention deficit/hyperactivity disorder (ADHD).20,21 As mentioned earlier, Western diets along with a lack of fruits and vegetables are associated with some mental disorders. These diet patterns lack omega-3 fatty acids, B vitamins, minerals, and amino acid precursors of neurotransmitters.22–24 These components act as antioxidants, anti-inflammatories, and precursors for neurotransmitter production. Many micronutrients, such as zinc, magnesium, and B vitamins including folic acid, and vitamin D, play a significant role in producing antidepressant effect.25–29 Experimental observations and some meta-analyses indicate that vitamin D supplementation can reduce the intensity of depressive disorders.30–32
The common mental health disorders and nutritional influence
Depression
A randomized, controlled study done in 2014 found that increasing omega-3 intake can reduce inflammation and prevent depression. Major depression includes decreased mood, increased sadness and anxiety, loss of interest in group activities, and sometimes loss of appetite. These patients are at high risk, as they have a significantly elevated likelihood of suicidal behavior.33 Psychotherapy, along with some antidepressants, is generally given to them.34 Tryptophan and tyrosine, amino acids obtained from protein, are precursors of various neurotransmitters, e.g., serotonin, dopamine, noradrenaline, and GABA (Gamma-Aminobutyric Acid), deficiencies of which cause depression.35–37 Another amino acid, methionine, in combination with ATP, produces S-adenosylmethionine, which helps produce neurotransmitters in the brain.38,39
Omega-3 fatty acids, including eicosa-pentaenoic acid and docosa-hexaenoic acid, present in fish and fish oil, have anti-depressive effects in humans.40 In addition, vitamin B (e.g., folic acid) and the trace metal magnesium have been shown to exhibit anti-depressive effects.41–44 Randomized, controlled trials exhibit decreased depression symptoms after administration of folic acid and magnesium in the diet.42,43
In brief, mechanistically, omega-3 fatty acids enhance brain function and reduce inflammation, linked to improved mood. B vitamins support neurotransmitter synthesis; deficiencies can lead to mood disorders. Vitamin D regulates mood and may reduce depressive symptoms; sunlight exposure is beneficial. Magnesium plays a role in neurotransmitter function; low levels are associated with increased anxiety and depression.45 Zinc is an important trace metal for brain health; supplementation may improve mood and cognitive function.46 Amino acids are the building blocks of neurotransmitters; adequate intake supports serotonin and dopamine production.47
Nutrients and their mechanism of action on anxiety, including OCD
Omega-3 fatty acids found in fish and flaxseeds support brain health and reduce anxiety symptoms. Magnesium, a trace metal, helps regulate neurotransmitter levels in the body and can alleviate stress. It can be found in leafy greens and nuts. Vitamin B is essential for energy production and brain function and can improve mood; it is found in whole grains and legumes. Probiotics maintain gut health, which is linked to mental health. Fermented foods like yogurt can enhance gut flora and reduce anxiety. Foods rich in antioxidants, such as berries and dark chocolate, combat oxidative stress and support mental well-being. Furthermore, adequate hydration is crucial for cognitive function.
OCD, which is also a type of anxiety disorder, is followed by stressful thoughts and compulsions.48 It is well documented that nutrients, like protein, which increase serotonin levels, help patients with OCD.49,50
Nutrients to address ADHD
Nutrients and their mechanisms of action to help ADHD are listed below. Omega-3 fatty acids support brain health and may improve attention and behavior. The trace metal zinc is essential for neurotransmitter function and can reduce ADHD symptoms. Another trace metal, iron, at low levels, can affect dopamine production; supplementation may help improve focus and cognitive function. The mineral magnesium plays a role in neurotransmission; adequate levels may help reduce hyperactivity. Vitamin D, at low levels, has been linked to increased ADHD symptoms. Vitamin B, particularly B6 and B12, supports energy metabolism and neurotransmitter synthesis, potentially aiding focus.21
Nutrients to address 617 bipolar disorder
Bipolar patients generally show depression, mania, and melancholy. Biochemically, these patients exhibit excessive acetylcholine receptors and elevated levels of vanadium.51,52 Vitamin C and its food sources, such as citrus fruits, have been shown to protect the body from vanadium-induced effects.53
Taurine, made from another amino acid, cysteine, in the liver, exhibits a calming effect on the brain. A deficiency of this amino acid may increase symptoms of bipolar mania.54 Further, low levels of omega-3 also contribute to the onset of bipolar symptoms.55 Omega-3 fatty acids support brain health and may reduce mood swings, whereas B vitamins are essential for neurotransmitter function and energy metabolism; deficiencies can exacerbate symptoms. Low levels of vitamin D are linked to mood disorders; supplementation may enhance mood. Trace metals, magnesium and zinc, help regulate anxiety and depression and may improve mood stability. Amino acids are the building blocks of neurotransmitters and support overall mental health.
Mechanistically, omega-3 fatty acids support brain health and may reduce mood swings. B vitamins are essential for neurotransmitter function; deficiencies may exacerbate symptoms. Low levels of vitamin D can cause mood disorders. Trace metal magnesium can alleviate anxiety and depression symptoms, whereas zinc plays a role in neurotransmission and improves mood stability. Amino acids are the building blocks of neurotransmitters, and adequate intake supports mental health.
Nutrients to control schizophrenia
Schizophrenia is a mental disorder that disrupts normal perception. Victims, generally during adolescence, may be paranoid and suffer from hallucinations, delusions, and impairments in speech and thinking abilities.56 Abnormal amino acid metabolism has been implicated in the onset of schizophrenia. Specifically, a low level of serotonin in the central nervous system has been correlated with schizophrenia.57–59
Administration of high doses of glycine (∼30 g) can reduce schizophrenia symptoms.60 Eicosa-pentaenoic acid, found in fish oils, has been shown to help with depression in schizophrenic patients.61,62 As mentioned earlier, omega-3 fatty acids support brain health and can reduce schizophrenia symptoms. Deficiencies of vitamins B and D can exacerbate schizophrenic symptoms; supplementation may improve mood and cognition. Antioxidants combat oxidative stress, which is implicated in schizophrenia pathology. Amino acids are precursors to neurotransmitters; adequate intake may help balance brain chemistry. Minerals, like zinc and magnesium, play roles in neurotransmission and may alleviate symptoms when supplemented. The above studies clearly indicate the what, why, and how of nutritional supplements in managing various mental disorders. Table 1 shows the psycho-protective effects of various bioactive components,63–69 such as vitamins, minerals, and omega-3, present in different kinds of foods.
Psycho-protective effects of the bioactive components found in foods
| Bioactive ingredients | Effects |
|---|---|
| Folate (Vit B9) | Prevent migraine, especially in patients with high homocysteine and a specific gene mutation63 |
| Omega-3 fatty acid | Stimulates neurotransmission, verbal and non-verbal communication processes64 |
| Flavonoids | Increases brain-derived neurotrophic; factor (BDNF) secretion, and reduces the patho-mechanism of depression65 |
| Exogenous amino acid – tryptophan | Forms serotonin that regulates the diurnal rhythm and emotional state66 |
| Micronutrients (Mg, Ca, Se, Zn, Mn, Cu, Vits. D, E, C, A) | Reduces oxidative stress, inflammation along with a decrease in C-reactive protein (CRP), interleukin-6 (IL-6), white blood cells (WBC), and psychological symptoms in a depressed condition67 |
| Complex carbohydrates, Eicosapentaenoic acid, Amino acid (glycine), Polyphenols, Anthocyanins | Regulates the neuromodulator and neurotransmitter expression, synaptic plasticity and activation of microglia68; Prevents inflammation and oxidative stress through inactivation of lipid peroxidation, and activation of catalase and superoxide dismutase69 |
Importance of gut-brain axis in psychiatric issues
The gut-brain axis involves the bidirectional relationship between the gastrointestinal biome and the central nervous system.70 The microbiota can also produce various neurotransmitters, such as butyric acid, γ-aminobutyric acid, serotonin, and dopamine. Furthermore, short-chain fatty acids have positive effects on mental disorders, including anxiety and depression.71,72 The psycho-protective effects of probiotics are shown in Table 2.73–76
Psycho-protective substances found in probiotics
| Bioactive ingredients in foods | Biological effects |
|---|---|
| Lactobacillus acidophilus Rosell-52; Bifidobacterium longum Rosell-175 | Healthy adults, blinded, randomized study: Reduces stress; Reduces depression and anxiety73 |
| Lactobacillus fermentum; Lactobacillus plantarum; Bifidobacterium lactis; Lactobacillus acidophilus; Bifidobacterium bifidum; Bifidobacterium longum | In Alzheimer’s disease: Probiotic consumption and also with selenium for 12 weeks had a positive effect on cognitive function74,75 |
| Lactobacillus plantarum C29 + powdered fermented soybeans (DW2009); Bifidobacterium breve A1 | In cognitive dysfunction: Oral supplementation of DW2009 and B. breve A1 can improve cognitive function in people with mild cognitive impairment (MCI)76 |
Effects of different diets on several mental issues
A comparative overview of brain-healthy dietary patterns, like Mediterranean (MD), Dietary Approaches to Stop Hypertension, Mediterranean-Dietary Approaches to Stop Hypertension, and Ketogenic diets—and their key components, proposed mechanisms of action, and neurological relevance—is shown in Table 3.77
Comparative overview of brain-healthy dietary patterns—MD, DASH MIND, and the Ketogenic diets
| Dietary pattern | Food components | Mechanism of action | Clinical significance |
|---|---|---|---|
| Mediterranean diet (MD) | High amounts: Fruits; Vegetables; Legumes; Whole grains; Nuts, olive oil. Moderate amounts: Fish and; Poultry meat; Low red meat and sweets | Antioxidant and anti inflammatory functions; Provides omega 3; Supports vascular health | Reduce the risk of depression, cognitive decline, and Alzheimer’s disease |
| Dietary approaches to stop hypertension (DASH) diet | High amounts: Fruits; Vegetables; Whole grains; Nuts, Olive oil; Fish and; Poultry meat. Low amounts: Sodium and; Sugars | Improves: Vascular functions; Metabolic functions; Supports cognitive stability | Mainly for the control of hypertension; Improve the brain-health in ageing populations |
| Mediterranean-DASH (MIND) diet | Combines elements of the Mediterranean and DASH diet | Antioxidant and anti- inflammatory functions. | Slower cognitive aging Reduce the risk of Alzheimer’s disease |
| Ketogenic diet | High amounts: Fat; Vegetables; Legumes; Whole grains; Nuts, Olive oil. Moderate amounts: Protein. Low amounts: Carb | Enhances mitochondrial functions; Reduces neuro-inflammation; Modulates brain-energy metabolism | Shows promise in: Epilepsy; Mood disorder; Neurodegeneration |
Clinical and public-health implications
Nutritional psychiatry is an emerging field that explores the relationship between diet and mental health. Research focuses on dietary patterns, gut microbiome health, and the impact of individual nutrients on mental health. This clinical feature article reviews evidence supporting nutritional interventions for mental health and provides clinical guidance. Applied psycho-pharmacotherapy or psychotherapy does not always yield the desired outcomes in treating mental disorders, warranting alternative interventions. Recently, research has increasingly focused on the nutritional impacts on mental health, highlighting its potential role in preventing various mental disorders. A recent review by Dighriri et al.78 seeks to determine the extent to which lifestyle and dietary factors influence mental health and assess the scientific evidence linking diet to mental well-being. Given current trends such as globalization and shifts in lifestyles and eating habits, it is logical to consider the complex connections among various factors and their effects on mental health in relation to the management of mental disorders, both therapeutically and preventively.
Mediterranean interventions appear to have substantial potential for alleviating depressive symptoms in people experiencing major or mild depression. However, to establish robust recommendations, there remains a need for high-quality, large-scale, and long-term randomized controlled trials.79 Our results indicate that a Mediterranean diet–based nutritional intervention enriched with extra virgin olive oil, in addition to usual treatment, compared with usual care without nutritional intervention, did not show efficacy regarding relapse prevention but might significantly reduce sub-syndromal depressive symptoms in patients with remitted major depression.
As far as we know, no previous studies have assessed the effect of a Mediterranean diet-personalized intervention added to usual care on reducing sub-syndromal symptoms in patients recovered from depression. Moreover, worldwide, this is the first long-term evaluation of a dietary intervention (follow-up and intervention period of two years) carried out in this type of patient. In this sense, we observed that the efficacy of the Mediterranean diet intervention on sub-syndromal symptoms of depression was maintained over time. For that reason, Mediterranean diet nutritional interventions, which are safe and inexpensive, seem to be a great tool for secondary depression prevention if their preventive properties are confirmed in future clinical trials in major depressive disorder.80
Epidemiological studies have shown that food components have either beneficial or adverse impacts on mental health.72 The challenge for “nutritional psychiatry” depends on evidence-based research to define the specific role of diet and nutrients on different aspects of mental health.81–83 One such study, to date, reported a significant improvement in mood and depression after 12 weeks with a Mediterranean diet in adult humans.84 More recently, a randomized controlled trial, Health and Life Sciences Integrated Medical Solutions, which is a Mediterranean-style dietary intervention supplemented with fish oil, and the PREDI_DEP trial (Prevention of Diabetes in People with Pre-diabetes), the first ongoing randomized clinical trial designed to assess the role of the Mediterranean diet in the prevention of recurrent depression, have confirmed these results.84,85
In contrast, the MooDFOOD trial (a double-blind randomized controlled trial designed to investigate the feasibility and effectiveness of nutritional strategies in the prevention of major depressive disorder) found that neither multi-nutrient supplementation nor food-related behavioral activation therapy reduced major depression in overweight or obese adults with depressive symptoms over one year, indicating that these specific nutritional and behavioral strategies may not be effective for preventing major depressive disorder in this population.86 This study suggests that a multi-nutrient supplement of omega-3 polyunsaturated fatty acids, vitamin D, folic acid, and selenium showed no significant reduction in depressive or anxiety symptoms, nor any improvement in health utility indices compared to a placebo.82 Randomized controlled trials and meta-analyses on vitamin D supplementation did not show improvements in depression among patients.87
A systematic review and meta-analysis of long-term supplementation with folic acid, vitamin B6, and vitamin B12 did not show any significant effect on the risk of developing depression in older men and women compared to a placebo group.88 Further, the vitamin B combination did not reduce the incidence or severity of depressive symptoms in older adults.88 Likewise, although there is an association between low selenium levels and depression, selenium supplementation generally did not show significant benefit for mood disorders in older adults, possibly due to the brain’s unique selenium storage.89 Multiple studies confirm that a high-quality diet in adulthood is associated with a reduced risk of cognitive decline, dementia, and Alzheimer’s disease. Diets rich in fruits, vegetables, nuts, legumes, and seafood are linked to better brain health, while diets high in red and processed meats, refined sugars, and added salt are associated with a greater risk of cognitive impairment. Alternatively, adherence to the Mediterranean diet or the Dietary Approaches to Stop Hypertension (DASH) shows a protective effect on cognitive function.90
Additionally, the consumption of antioxidant polyphenols is linked to improved cognitive ability in older adults, as evidenced by studies showing that higher polyphenol intake can lead to better cognitive performance and reduced dementia risk. These beneficial effects are thought to stem from polyphenols’ ability to reduce oxidative and inflammatory stress in the brain, activate neuro-protective pathways, and potentially promote synaptic plasticity and neurogenesis.91 A randomized clinical trial with a Mediterranean diet supplemented with nuts or extra virgin olive oil showed that older adults with cardiovascular risk exhibited improved cognitive function, including memory and global cognition, compared to a low-fat diet. Participants in the Mediterranean diet groups performed better on tests of memory, attention, speed of thought, and executive function.92
Mental illnesses are associated with numerous metabolic disorders, such as obesity, diabetes, and cardiovascular disease. A cluster of metabolic syndromes, including abdominal obesity, high blood pressure, high blood sugar, and high triglycerides, is found in people with abnormal mental health conditions.93 The ketogenic diet is an evidence-based treatment for epilepsy that works by altering brain metabolism and neurotransmitter function to stabilize neuronal activity and reduce seizures.94,95 By providing ketone bodies as an alternative brain fuel to glucose, the ketogenic diet enhances GABAergic (inhibitory) neurotransmission, reduces glutamatergic (excitatory) neurotransmission, and improves mitochondrial function, all contributing to a decrease in seizure frequency.96,97 A study by Shin et al.98 on the ketogenic diet and epilepsy indicated that 36% of 14 children (approximately five children) had a >50% reduction in seizures, and 12% (approximately one to two children) became seizure-free. This does not match the user’s data of 10 patients with >50% reduction and seven being seizure-free.98,99
Limitations of this type of studies
Our studies depend solely on published databases. Hence, many studies rely on self-reported dietary intake, which can be inaccurate. Further, the sample sizes are often small, limiting the generalizability of findings, and there is also a lack of standardized methods. On top of that, variables such as lifestyle and socioeconomic status are frequently overlooked. Nutritional interventions, in reality, are difficult to standardize across diverse populations. Further, the complexity of mental disorders makes it challenging to isolate an experimental group for the evaluation of dietary effects from other factors.
Conclusions
Overall, the present review indicates that advances in nutritional psychiatry are crucial for preventing and treating mental health disorders, but require more replicated, refined, and scaled-up dietary intervention studies, particularly randomized controlled trials, to establish acceptable evidence for nutrition’s role in mental well-being. In short, mental diseases like depression, anxiety, and many others are leading health issues worldwide. Although each can be treated and addressed differently, research shows that nutrition plays a huge role in all of them. The Western diet can promote inflammation, and inflammation which can cause anxiety, stress in the body, whereas MIND (Mediterranean-DASH), as they are rich in fruits, vegetables, whole grains, and omega-3, supply antioxidant and anti- inflammatory substances, which can counteract the effects of inflammation and may alleviate anxiety and stress symptoms. Many micronutrients, such as zinc, magnesium, and B vitamins including folic acid, and vitamin D, play a significant role in producing an antidepressant effect. The gut-brain axis involves the bidirectional relationship between the gastrointestinal biome and the central nervous system. The psycho-protective effects of probiotics are therefore important for restoring gut homeostasis. In addition, staying hydrated can promote digestive function, and regular physical activity enhances gut motility. However, the complexity of mental disorders makes it challenging to isolate an experimental group for the evaluation of dietary effects from other factors. Figure 1 provides a comprehensive overview of these interconnected factors and their roles in mental health.
Declarations
Acknowledgement
We acknowledge all our staff members and scientists from Sacred Heart University, Fairfield, CT, Chemistry Department, as well as St. John’s University, Queens, NY, Education Department, for their support during the writing of this review by providing materials and editing. We also acknowledge Mrs. Joyana Rosenthal, Empowerly, for editing the manuscript.
Funding
No funding was received from any source for this project.
Conflict of interest
The views expressed in this article are solely those of the authors and do not reflect the official policy of the Institutions. The authors declare no conflict of interest, financial or otherwise.
Authors’ contributions
Information search, writing of the manuscript, and visualizing the concept (AC, SG, SB). All authors have approved the final version and publication of the manuscript.

 Author information
Author information