Introduction
As refractive cataract surgery increasingly becomes the standard approach, corneal astigmatism is progressively recognized as a significant factor influencing postoperative visual quality for cataract patients.1 Astigmatism is a prevalent refractive error characterized by an abnormal curvature of the cornea or lens, and it frequently occurs concurrently with cataracts. This ocular irregularity alters the focal convergence of incoming light, resulting in vision that is blurred and distorted, affecting the clarity of both near and distant objects.1 Within the cataract-afflicted demographic, the incidence of astigmatism is clinically noteworthy, as it may exacerbate refractive inaccuracies post-cataract surgery. The occurrence of astigmatic aberrations among patients with cataracts varies among different population subsets; however, research indicates its considerable presence, with a significant fraction of those awaiting cataract surgery exhibiting moderate to severe astigmatism.1 The convergence of these two visual impairments demands a sophisticated surgical strategy that not only resolves the opacification typical of cataracts but also corrects the corneal distortion associated with astigmatism. Adopting an integrative approach is crucial for optimizing visual outcomes and enhancing patient satisfaction.2,3
As a result, devising strategies for astigmatism correction has emerged as a current challenge for cataract surgeons. Presently, surgical procedures for combining cataract removal with astigmatism correction include limbal relaxing incisions,4 arcuate keratotomy (AK),5 and the use of toric intraocular lens implants (TIOL).6 Among these, manual AK serves as an effective and cost-efficient strategy for correcting corneal astigmatism. However, the incisions produced by this method offer low repeatability and predictability, presenting a risk of corneal perforation and variable correction results.7 The advent of femtosecond laser-assisted cataract phacoemulsification has led to growing interest in the use of femtosecond lasers for creating arcuate incisions in the cornea (femtosecond arcuate incisions),8 also known as the femtosecond laser-assisted arcuate keratotomy (FSAK) procedure.
FSAK performs arcuate incisions on a predetermined corneal meridian with the support of a digital navigation system.9 It leverages the conjugate effect of flattening the steep axis of corneal astigmatism and enhancing the flat axis to correct the astigmatism. It permits personalized correction for each patient’s corneal astigmatism by varying surgical parameters such as the length of the arc, depth, and diameter of the incision, and deciding whether or not to cut the corneal anterior surface.10 The advent of FSAK has amplified the safety and effectiveness of AK astigmatism correction, showcasing impressive long-term stability.8 Femtosecond laser-assisted corneal arcuate keratotomy represents a precise, long-term, and safe surgical intervention for the correction of low to moderate astigmatism. However, it requires careful consideration of corneal biomechanics and individual healing variations, with ongoing research needed to refine techniques and maximize patient outcomes. This paper intended to provide a comprehensive review of the research on FSAK.
FSAK’s correction range for corneal astigmatism
Wortz et al.11 evaluated the actual effect of FSAK in correcting mild corneal astigmatism (< 1.00 D) by applying a new arcuate incision calculation formula. They found that the number of patients in the FSAK group with postoperative corneal astigmatism equal to or less than 0.50 D was 3.2 times higher than in that of the standard surgery group, and the number of patients whose vision reached 0.8 or more was 3.54 times higher. Therefore, they concluded that well-designed FSAK using improved surgical design charts can achieve excellent anatomical and refractive correction results. In a retrospective cohort study, Baharozian et al.12 revised and improved the commonly used Donnenfeld’s Chart for femtosecond laser corneal surgery. They found that FSAK had a certain corrective effect on corneal astigmatism of ≤ 1.25 D. Wendelstein et al.13 used the Castrop Chart to evaluate the correction effect for corneal astigmatism ranging from 0.70 to 2.50 D and obtained effective and stable results. Studies also suggested that FSAK can effectively correct mild and moderate astigmatism.14 Schwarzenbacher et al.15 used low-energy femtosecond laser devices to create penetrating FSAKs and correct mild to moderate astigmatism. The results showed that one year after the surgery, this procedure effectively and consistently reduced preoperative corneal astigmatism from an average of 1.50 D to 0.50 D. In conclusion, FSAK can correct mild to moderate corneal astigmatism. However, the corrective effect and stability for high astigmatism remain to be evaluated.
Configuration of surgical parameters for FSAK
The differences in the settings of various surgical parameters result in disparities in keratoconus correction outcomes, while also facilitating customized surgical designs by exploiting these correctional disparities. Comparing the correction effects of different surgical parameter settings is a focal point of the research. Variables like the incision depth of FSAK, the distance from the incision to the corneal edge, and the openness of the penetrating FSAK can influence the outcomes of astigmatic correction to varying extents.16
Incision depth
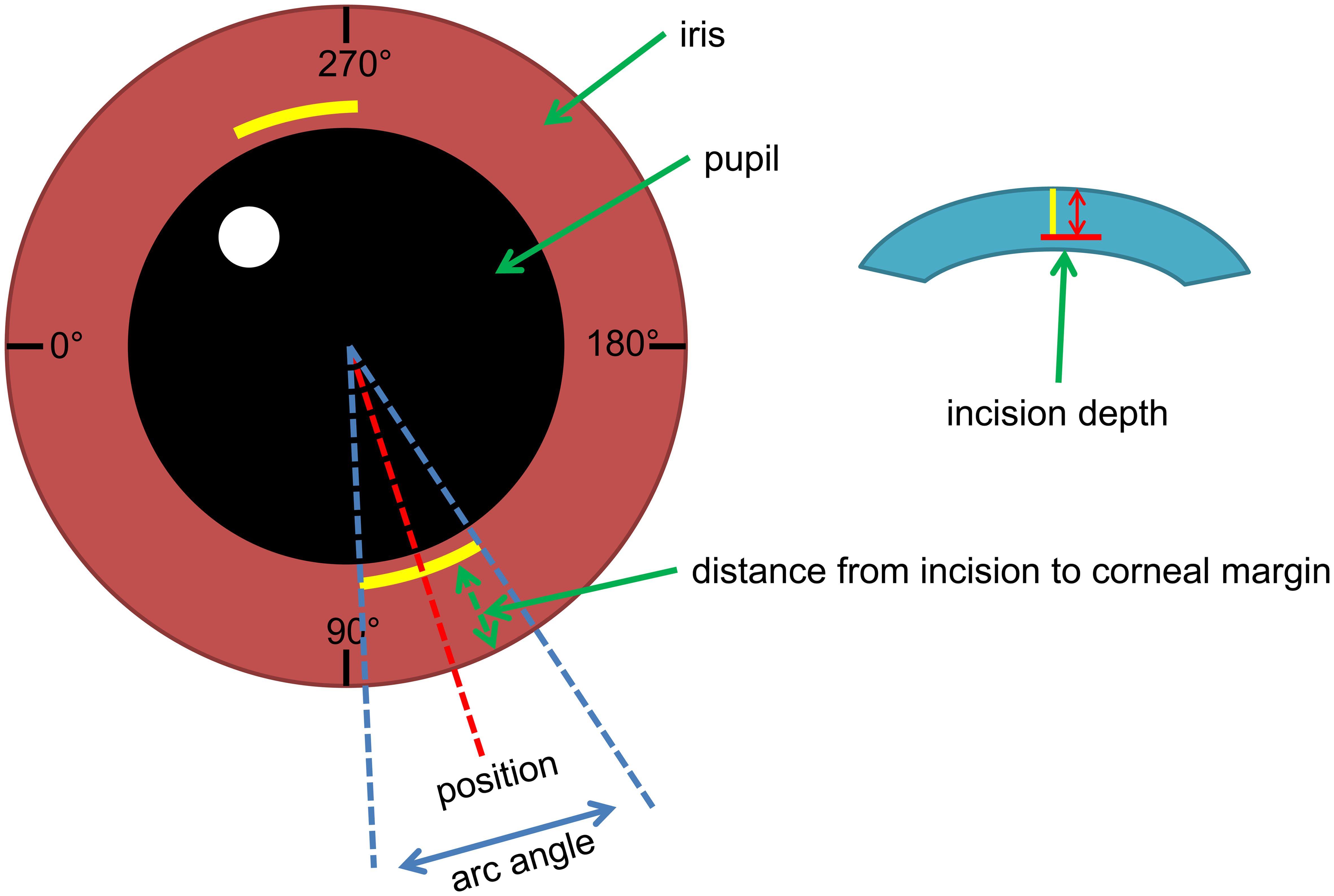
Figure 1 illustrates the surgical parameters for FSAK. In a prospective study conducted by Nejima et al.17 data analysis was performed on the incision depth measured by Anterior Segment Optical Coherence Tomography (OCT). They constructed a scatter plot charting the relationship between the depth of the incision as measured by the anterior segment OCT one month post-surgery and the predetermined depth of the incision. They observed that all measured depths of incision exceeded the projected values. Typically, femtosecond lasers can create incisions with a high degree of precision, and it is generally observed that incisions based on accurate data tend to reach the expected depth. Therefore, they hypothesized that the greater measured depth of incision could have resulted from leveling intensity and other settings linked to the femtosecond laser. However, as the sample size in this study was confined to as few as six patients (with a total of eight eyes), the conclusions require further verification.
Distance from incision to corneal margin
Studies show that, when the same incision diameter and similar operative design parameters are applied, Asians have poorer astigmatism correction effects when using FSAK compared to Caucasians.18 Hickson-Curran et al.19 found that anatomical parameters of the cornea in Asians differ from those in Caucasians, with the average corneal diameter in Asians being 0.5 mm smaller. Zhang et al.8 discovered that, under the same FSAK parameter settings, the smaller corneas of Asians result in incisions closer to the corneal margin, potentially reducing the impact of incisions on the biomechanical properties of the cornea and thereby diminishing the effect of astigmatism correction. A Pearson correlation analysis on the distance from FSAK to the corneal margin and the FSAK arc length found a significant correlation between the distance from FSAK to the corneal margin and the size of surgically induced astigmatism (SIA). They measured the vertical corneal diameter of the patients (10.67 ± 0.62 mm), noting it to be noticeably smaller than the horizontal corneal diameter by 0.81 mm. Thus, the closer proximity of FSAK to the corneal margin in the with-the-rule astigmatism group might result in diminished astigmatism correction effects. This may explain why similar FSAK yields greater astigmatism correction effects in the against-the-rule astigmatism group. While the aforementioned studies conclude that the distance from the incision to the corneal margin can serve as an independent factor affecting SIA, related studies are relatively few, and further validation is required. Zhang et al. investigated the effectiveness of epithelium- and Bowman’s membrane-penetrating FSAK for correcting preoperative astigmatism in cataract patients. Their findings highlighted that the distance from the incision to the limbus serves as a significant independent predictor of SIA.8
Blunt dissection of penetrating FSAK
Blunt dissection to open the arcuate incision can be performed during or after penetrating FSAK surgery. Chan et al.20 pointed out that opening the penetrating FSAK can enhance the flattening effect of FSAK. Visco et al.21 believe that the full refractive effects of FSAK are only exhibited when it is opened. Some surgeons advocate for partial preservation or no blunt dissection of the cut during cataract surgery, opting instead to open the cut under a slit lamp microscope postoperatively based on the astigmatism correction effect. Hernandez et al.22 open the FSAK before the end of the operation. Although a fully open FSAK requires a longer healing time, it has a more apparent astigmatic correction effect compared to other studies. Consequently, opening the FSAK through blunt dissection can enhance the astigmatism correction effect.
Effectiveness of FSAK compare with other surgeries
Comparison of the effects of FSAK and manual corneal relaxing incision
Prior to the advent of FSAK, AK incisions were typically made manually with a corneal knife to correct corneal astigmatism. However, as mentioned above, the reproducibility of manually made AK incisions is poor. Additionally, they pose risks of postoperative corneal expansion and inward growth of the corneal epithelium.5 Mayer et al.23 found no significant differences in the inflammatory reaction surrounding FSAK and manually made corneal incisions in their study on the ultrastructure of corneal incisions. However, FSAK demonstrated noticeably more cytoapoptosis (death of corneal cells), which could potentially affect the healing of the postoperative corneal incision. Compared to manually made corneal incisions, FSAK shows higher structural stability and reproducibility. A parallel comparison of the corrective effects reveals that Roberts et al.24 found that FSAK has a higher correction index (CI), implying that FSAK could better correct corneal astigmatism than manually made corneal incisions. The results of a study using vector analysis also suggested that manually made corneal incisions primarily influence the correction of oblique astigmatism, but less so with the correction of either with-the-rule or against-the-rule astigmatism, while FSAK works to correct all three.24 Therefore, it may be concluded that FSAK is more effective than manual AK incisions in correcting corneal astigmatism.
Comparison of the effects of penetrating and intrastromal FSAK
Femtosecond lasers can produce penetrating FSAKs that pass through the front surface of the cornea and intrastromal FSAKs that do not penetrate the corneal front surface. Since commonly used femtosecond laser devices do not completely separate tissues during cutting but leave microbridges, some researchers suggest that blunt dissectors are needed to open incisions in penetrating FSAKs, while others disagree. This discrepancy may be a source of variability in SIA.25 Intrastromal FSAKs, which have intact Bowman’s and Descemet’s membranes, are considered more stable. Zhang et al.8 found higher CIs in their research on penetrating FSAK. Day and Stevens conducted research on intrastromal FSAK and found that changes in SIA were approximately 0.1 D during the postoperative follow-up of one to six months.26 Although these differences were statistically significant, they were not necessarily clinically meaningful. Furthermore, a study by Nubile et al.27 on the healing process of penetrating FSAKs found that the incisions initially exhibited inward epithelial growth followed by the formation of fibrotic scars, potentially leading to postoperative refractive instability. Therefore, compared to penetrating FSAKs, intrastromal FSAKs are more stable, and their clinical astigmatism corrective effects are significant. However, compared to penetrating FSAKs of the same diameter and arc length, the CIs of intrastromal FSAKs are comparatively lower.28
Comparison of FSAK and TIOL implantation
The implantation of TIOLs is also a commonly used and effective method for astigmatism correction. However, studies have demonstrated that any rotation or misalignment of a TIOL by just 1 degree results in a 3.3% reduction in the artificial lens’ cylindrical refractive power, making the postoperative axial stability of TIOLs critical.22,29 Although postoperative rotation and misalignment of implanting TIOLs can lead to complications, TIOL implantation requires no additional incisions compared to AK surgery and thus avoids weakening the corneal structure.30 A study comparing the correction of cataracts and corneal astigmatism using manual corneal incisions, FSAK production, and TIOL implantation revealed that the TIOL implantation group showed better predictability, stability, and a higher average correction index than the FSAK group. Researchers speculate that this might be due to the lengthy healing time for FSAK, leading to a trend of corneal astigmatism regression in the later stage.31 A study by Hernandez et al,22 found no significant difference between the TIOL implantation and FSAK groups in terms of error angle, correction magnitude, and correction index. However, three months post-surgery, the equivalent spherical lens of the TIOL implantation group was closer to emmetropia compared to the FSAK group. In a recent domestic study comparing FSAK and TIOL implantation for the correction of cataracts and corneal astigmatism, it was discovered that the postoperative residual astigmatism one year after TIOL implantation was 0.260 ± 0.132 D, less than that of the FSAK group (0.417 ± 0.183 D). Visual acuity without eyeglasses was also superior in the TIOL group, with these differences achieving statistical significance. As a result, it is suggested that the long-term correction effect of TIOL implantation is superior to FSAK, providing better visual outcomes.32 TIOL implantation has been shown to produce superior results in the correction of moderate astigmatism. Nonetheless, femtosecond laser-assisted keratoplasty continues to be a reliable method for reducing astigmatic errors.22
Long-term correction effect after FSAK
Literature indicates that manual AK correction of corneal astigmatism can regress as the corneal incision heals, resulting in a longer time to reach stability.7 The long-term effect of FSAK is a focus of attention for clinical practitioners. Chan et al.33 in their follow-up study from two months to two years post-FSAK surgery, found that FSAK presents significant stability in correcting low to moderate corneal astigmatism. Furthermore, they discovered that the long-term correction effect of phacoemulsification cataract extraction combined with FSAK correction of astigmatism remained stable for two to five years postoperatively.33 A retrospective study found that individuals with a preoperative mean refractive astigmatism of 0.92 ± 0.34 D experienced stable postoperative astigmatism of 0.14 ± 0.23 D one year later, with 95.8% of patients having postoperative astigmatism ≤0.50 D, thus stabilizing the correction effect.34 A study in 2022 also found that FSAK could effectively improve vision stability six months postoperatively, making it a potentially effective method for correcting residual astigmatism following cataract removal or corneal transplantation surgeries.9 In summary, FSAK demonstrates relatively high stability in correcting astigmatism, with long-term corrective effects also appearing stable. However, due to the limited related research and data, further observation is needed regarding the stability of the long-term correction effect.
Limitations of FSAK
Dry eye
Research has reported that FSAK may cause dry eye. Day et al.35 found in their study on astigmatism correction with intrastromal FSAK that femtosecond laser cutting of corneal tissue may affect corneal nerves, leading to reduced nerve sensitivity near FSAK, resulting in secondary dry eye. Some studies have reported that a small number of patients developed typical dry eye symptoms, such as itching and a foreign body sensation, one-week post-operation, with treatment being administered using artificial tears, though the recovery outcomes remain unclear.36 There is relatively less research on dry eye induced by FSAK, warranting further relevant research and analysis.
Corneal perforation
Research on FSAK for the correction of corneal astigmatism has confirmed the safety of the procedure. However, there have been individual reports of intraoperative or postoperative perforation due to improper operation and low patient cooperation. Kymionis et al.37 reported a case of corneal perforation caused by FSAK. The analysis of surgical videos revealed that at the end of the surgery, bubbles formed within the anterior chamber of the operative eye when the FSAK was opened. This bubble formation, a characteristic of femtosecond laser cutting through corneal tissue, could be one of the causes of corneal perforation. Another report documented three cases. In the first case, the patient moved the operative eye while manually adjusting the femtosecond laser parameters, leading to a loss of suction and corneal cutting complications. In the second case, a shallow anterior chamber in the operative eye and loss of suction were not identified promptly during the procedure, leading to the laser cutting through the cornea. In the third case, due to the patient’s poor cooperation, a full-thickness corneal incision was formed at the designed incision location. Therefore, surgeons need to adjust the laser program promptly after docking to avoid the patient’s lack of focus and eye deviation, preventing complications.38
Corneal aberrations
Studies have indicated that FSAK may lead to alterations in corneal high-order aberrations. In a comparative study of FSAK and TIOL implantation, Lee et al.39 analyzed the high-order aberrations caused by both. The authors divided the participants into groups: those who underwent FSAK and femtosecond laser-assisted cataract surgery without FSAK, and a conventional cataract phacoemulsification (Phaco) group. Corneal aberration assessments indicated that the root mean square values of high-order aberrations and total trefoil in the FSAK group were significantly higher than in the Phaco group, while the corneal high-order aberrations for femtosecond laser-assisted cataract surgery without FSAK were not significantly different from the Phaco group. Chan et al.33 after operating arcuate incisions on the VICTUS femtosecond laser platform in Germany, found that two months and two years postoperatively, coma, trefoil, and total high-order aberrations significantly increased compared to preoperative measurements, while spherical aberration did not show significant differences. This suggests that the reduction of astigmatism is associated with an increase in high-order aberrations. However, Schwarzenbacher et al.,15 applying the new femtosecond laser platform LDV Z8 for arcuate incision creation in their research, discovered a significant reduction in total corneal high-order aberrations postoperatively, with no apparent alteration from one month to one-year follow-up, and even demonstrated an improvement. Spherical aberration increased one month postoperatively but declined to preoperative levels after three months and remained stable over the next nine months. Although FSAK may lead to changes in high-order aberrations, the varying equipment used for creating femtosecond laser arcuate incisions necessitates further research to properly evaluate these trends.
Furthermore, Kanclerz and colleagues conducted an analysis of the advantages and limitations of femtosecond laser-assisted cataract surgery compared to conventional phacoemulsification cataract surgery. Their findings indicate that femtosecond laser-assisted cataract surgery appears to offer benefits to specific patient cohorts, namely those with a low baseline endothelial cell count or individuals intending to undergo multifocal intraocular lens implantation. However, it has been acknowledged that the superiority of femtosecond laser-assisted cataract surgery is not unequivocal in every routine case. Consequently, its adoption cannot be universally advocated as being cost-effective.34
Challenges and prospect
Femtosecond laser-assisted corneal arcuate keratotomy is an effective, long-term stable, and safe procedure for correcting astigmatism. The integration of femtosecond laser technology with anterior segment OCT has enhanced the precision of keratotomy incision parameters and reduced the risk of intraoperative or postoperative complications. This advancement significantly contributes to correcting low to moderate astigmatism in preoperative cataract patients. However, this technique presents nuances and challenges. Accurate alignment and depth precision are crucial, as the femtosecond laser creates corneal incisions requiring meticulous control to avoid perforation and irregular astigmatism. Surgeons must adeptly consider corneal biomechanics and individual wound-healing responses to ensure predictable outcomes. Achieving the ideal optical zone size remains a delicate balance between effective astigmatic correction and the preservation of corneal integrity. Furthermore, this technology necessitates a deep understanding of astigmatic vector analysis to tailor patient-specific nomograms, posing a steep learning curve for ophthalmic surgeons. Due to the limited number of related studies, further comprehensive research is necessary to obtain more accurate incision parameters and more comprehensive surgical planning. This will provide a more reliable theoretical basis for improving patients’ postoperative visual quality and quality of life.
Conclusions
Femtosecond laser-assisted arcuate keratotomy represents a significant advancement in the field, providing improved correction of astigmatism and quality of life for cataract patients. Further advancements and studies are expected to hone the precision of this technique, ensuring safer and more effective outcomes.
Declarations
Acknowledgement
None.
Funding
None.
Conflict of interest
None.
Authors’ contributions
The sole author contributed everything to this manuscript.

 Author information
Author information